ibs insight guide
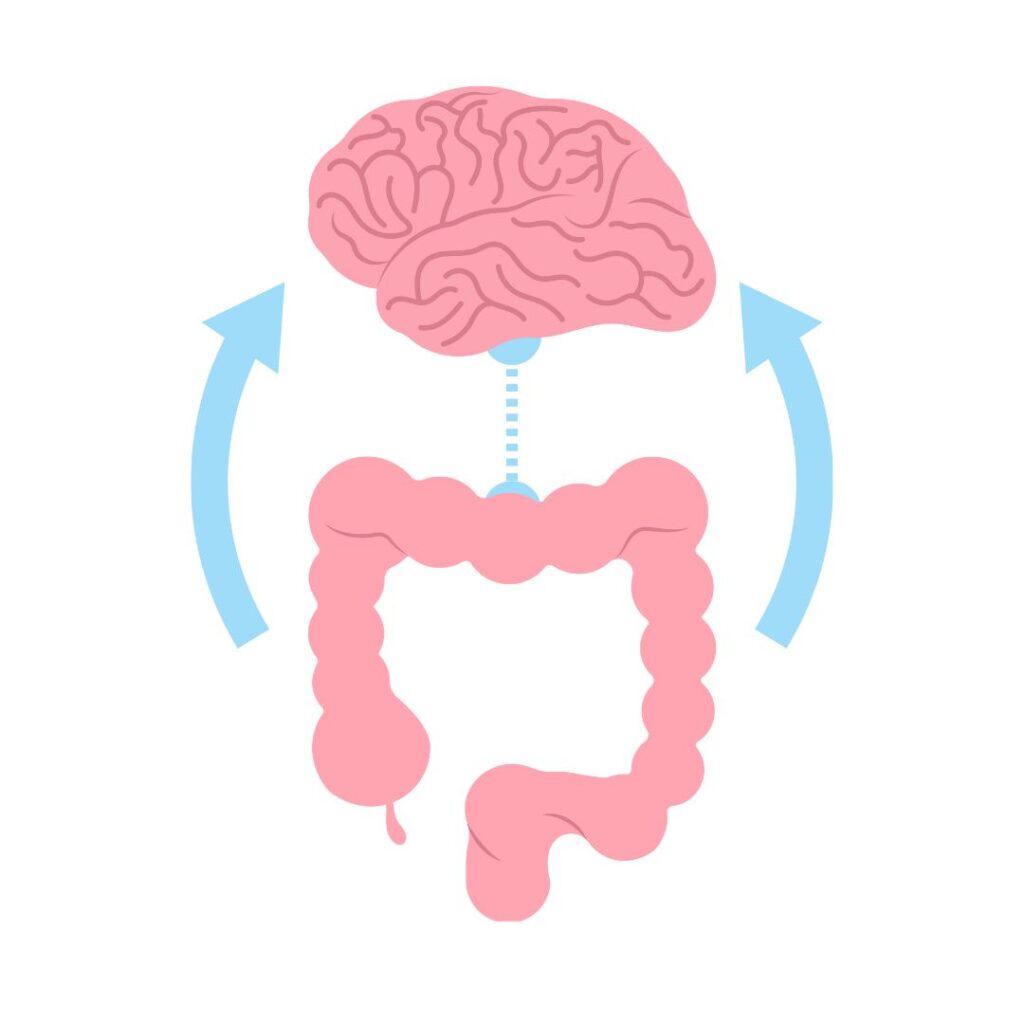
The Gut-Brain Axis and IBS: Why IBS is Considered a disorder of the Gut-Brain Axis

Irritable Bowel Syndrome (IBS) is increasingly recognized as a disorder of the gut-brain, meaning that it’s not solely a digestive issue but a condition involving complex interactions between your gut and brain. Here’s why understanding IBS as a gut-brain disorder is crucial:
1. The Gut and Brain Are Constantly Communicating via the vagus nerve, hormones and neurotransmitters: The gut-brain axis allows your gut and brain to continuously send signals back and forth. In people with IBS, this communication can be hypersensitive or easily disrupted. Stress, anxiety, or changes in the gut environment can trigger this axis to respond, leading to heightened pain sensitivity, bloating, and digestive symptoms.
2. Nervous System Sensitivity: In IBS, the nervous system often becomes more sensitive, responding intensely to minor triggers like certain foods, stress, or hormonal changes. This means that what might be a mild discomfort for someone without IBS can become a painful, full-blown symptom for someone with IBS due to heightened gut-brain communication.
3. Stress and Emotions Affect the Gut: IBS symptoms often worsen during stressful periods, not just because of digestive changes, but due to the brain’s influence on the gut. When stressed, your brain releases hormones that affect gut motility (how quickly food moves through the digestive system), inflammation, and the balance of gut bacteria—all of which can intensify IBS symptoms.
4. Microbiome’s Role in Gut-Brain Health: The gut microbiome—the community of bacteria living in the intestines—has a direct impact on gut-brain communication. Imbalances in the gut microbiome can lead to inflammation and even mental health symptoms like anxiety or depression, creating a cycle that worsens IBS.
5. Why IBS Needs a Mind-Gut Approach: Because IBS involves both the mind and body, it’s not enough to treat just the digestive symptoms. Cognitive Behavioral Therapy (CBT) and gut-directed hypnotherapy, for instance, help manage stress and regulate gut-brain communication, reducing symptom severity by addressing the root causes in the brain-gut connection.
Understanding IBS as a gut-brain disorder allows you to take control over more than just the physical symptoms—it empowers you to use mental and lifestyle approaches to regulate your body’s response, calming both mind and gut. This is the focus of my approach: giving you tools to manage IBS from a mind-gut perspective for long-term relief and improved quality of life.



